Improve Patient and Member Experiences with a Customer Data Platform

With the rise of digital health, telemedicine, retail healthcare, and consumerism, the ability to observe a 360-degree view of the customer is more essential than ever before. Moreover, with expanding value-based care models, healthcare organizations are experiencing increased pressure to measure and establish more accountability in process and technology. Yet, moving from disjointed and siloed experiences to connected end-to-end orchestrated journeys has proven challenging. To deliver on customer expectations and industry demands, many healthcare organizations are turning towards Customer Data Platforms (CDPs) to scale and leverage customer data more efficiently. The global healthcare customer data platform market size is expected to reach USD 1.6 billion by 2028.
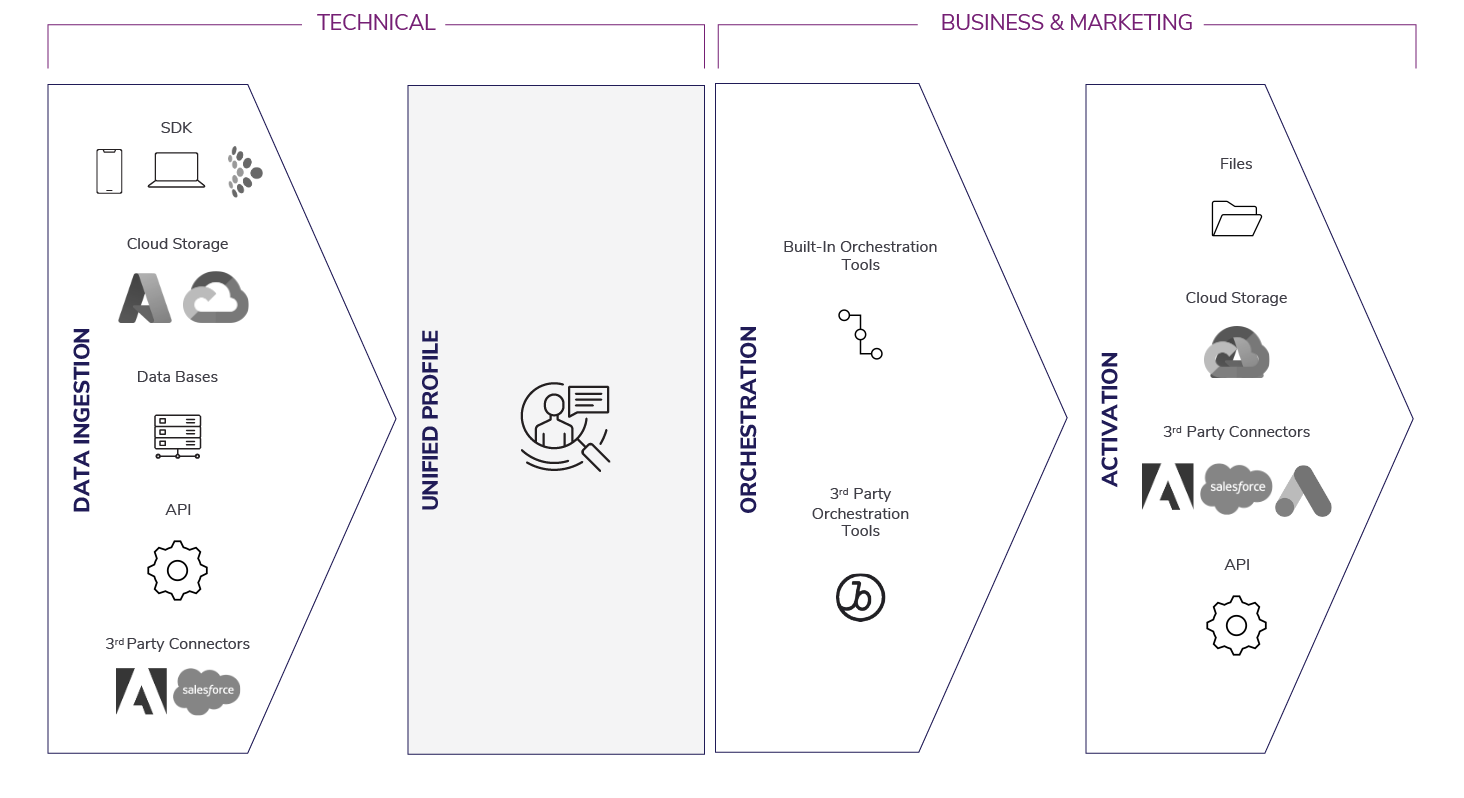
The CDP Institute defines a CDP as a packaged software that creates a persistent, unified customer database that is accessible to and enables other systems, including activation platforms such as email providers and social channels. CDPs create the foundation to develop connective experiences, and were created to solve for disconnected data, siloed operations, and visibility into the customer experience.
For payers and providers, CDPs offer a pathway towards identifying invaluable insights and opportunities to enhance patient care, streamline operations, and drive better outcomes. They create a single, trusted view of patient or member records that can be shared across the organization. With this customer profile in hand, marketing, sales, and customer service can all work together to drive relevant, personalized experiences across the care continuum.
It should be said that implementing a CDP shouldn’t feel like “just one more thing” for marketers and IT to manage. Instead, selecting and implementing a CDP can provide simplification for both teams, supporting governance controls and enablement within one solution. And of course, a CDP is more than just a re-marketing tool, it provides centralized audiences for orchestration and automation, and can be the technical catalyst that finally allows your organization to build the customer experience that you dream about.
Regardless of the chosen vendor or platform partner, a CDP should support or enable some combination of the following capabilities:
- Data streaming and centralized profile management
- Easily configured integrations (activation layer) with marketing applications within your ecosystem that will drive business outcomes including ROI, efficiencies, and improved customer experience
- Ability to support meaningful analysis, data science, or machine learning efforts
- Data storage, governance, and stewardship capabilities (to be supplemented by internal processes and ways of working)
- Infrastructure that provides HIPAA-ready features, or cloud architectures that assist in compliance with data privacy and regulatory requirements
Architecture remains the same when considering a payer or provider application, but use cases and applications may differ.
Empowering Payers to Reach Members
Payers are making significant investments in digital experience platforms and HIPAA-ready solutions to deliver 1:1 personalized and omni-channel experiences. By consolidating data from disparate sources, payers can create a unified profile of each member that enables customer journey orchestration, meaningful insights, and personalization capabilities to improve member acquisition, engagement, and retention.
Example Member Profile Within a CDP
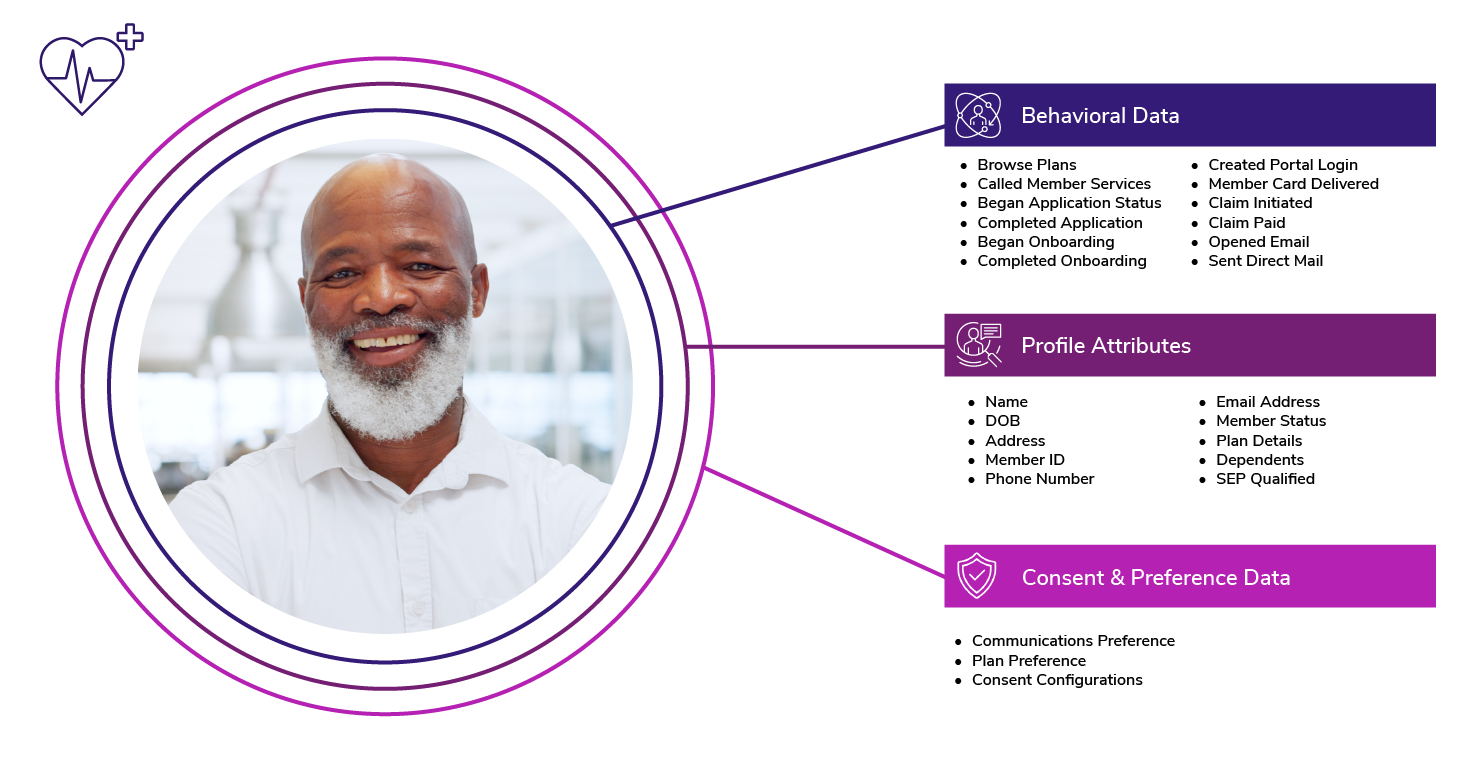
Member Acquisition and Registration
CDPs provide the audience and profile layer to improve shopping, pre-effective onboarding, and orientation activities. Opportunities include:
- Progressive profile building to deliver real-time messaging for insurance product awareness during digital-first shopping
- Coordinate an omnichannel strategy that delivers a consistent and cohesive narrative to prospects throughout their shopping journey and enrollments
- Identify members who may need more support during onboarding, providing alternate methods of communication and research to reduce call center volume
- Proactively engaging members with information that is most important to them prior to their new insurance taking effect
Member Engagement and Retention
Once a prospect becomes a member, CDPs improve member loyalty and retention, and provide compliance and process efficiencies. Opportunities include:
- Leverage SMS for “on hold” calls to let members know when they can complete their action online
- Increase employee awareness and engagement with available employer benefit programs to drive adoption and ROI
- Leverage member profile data and predictive analytics to send targeted, relevant messages through preferred channels
Enhancing Provider Performance
Likewise, healthcare providers can leverage CDPs in a similar way to elevate the quality and efficiency of care delivery. Key No-HIPAA use cases focus on driving impact to KPIs including awareness, acquisition, care plan adherence, reduction in re-admittance rates, journey campaign effectiveness, call center deflection, self-service enablement, and more.
Example Patient Profile Within a CDP (Marketing Focus, No HIPAA)

Patient Acquisition, Retention, and Engagement
CDPs provide the audience and profile layer to improve patients’ exposure to providers, including onboarding, finding care, and post-care adherence.
- Use patient preferences and attributes to deliver personalized and relevant recommendations for services and providers
- Encourage new patients to use self-service tools to complete intake activities ahead of their appointment (i.e. mobile app)
- Orchestrate regular outreach through preferred channels to educate and coach patients through their care regimen
- Detect when a patient or caregiver might be struggling to get the care they need and reach out through preferred channels
Applications Beyond Marketing and Sales
Because CDPs structure disparate data, healthcare organizations are presented with a unique opportunity to extend the use of CDPs past marketing efforts to improve the overall patient and member experience.
Improving Patient Outcomes
By aggregating patient data from various touchpoints, including clinical encounters, lab results, and medication histories, providers can gain deeper insights into each patient's medical history, preferences, and social determinants of health. Applications may include profile analysis to identify earlier intervention points for key diagnoses, improving patient outcomes, and decreasing readmission rates. Teams may also analyze profiles to understand the performance of critical care management strategies across their population to optimize outcomes. Providers may also proactively manage chronic conditions through targeted educational materials.
Example Profile Within a CDP (Clinical Focus, HIPAA)
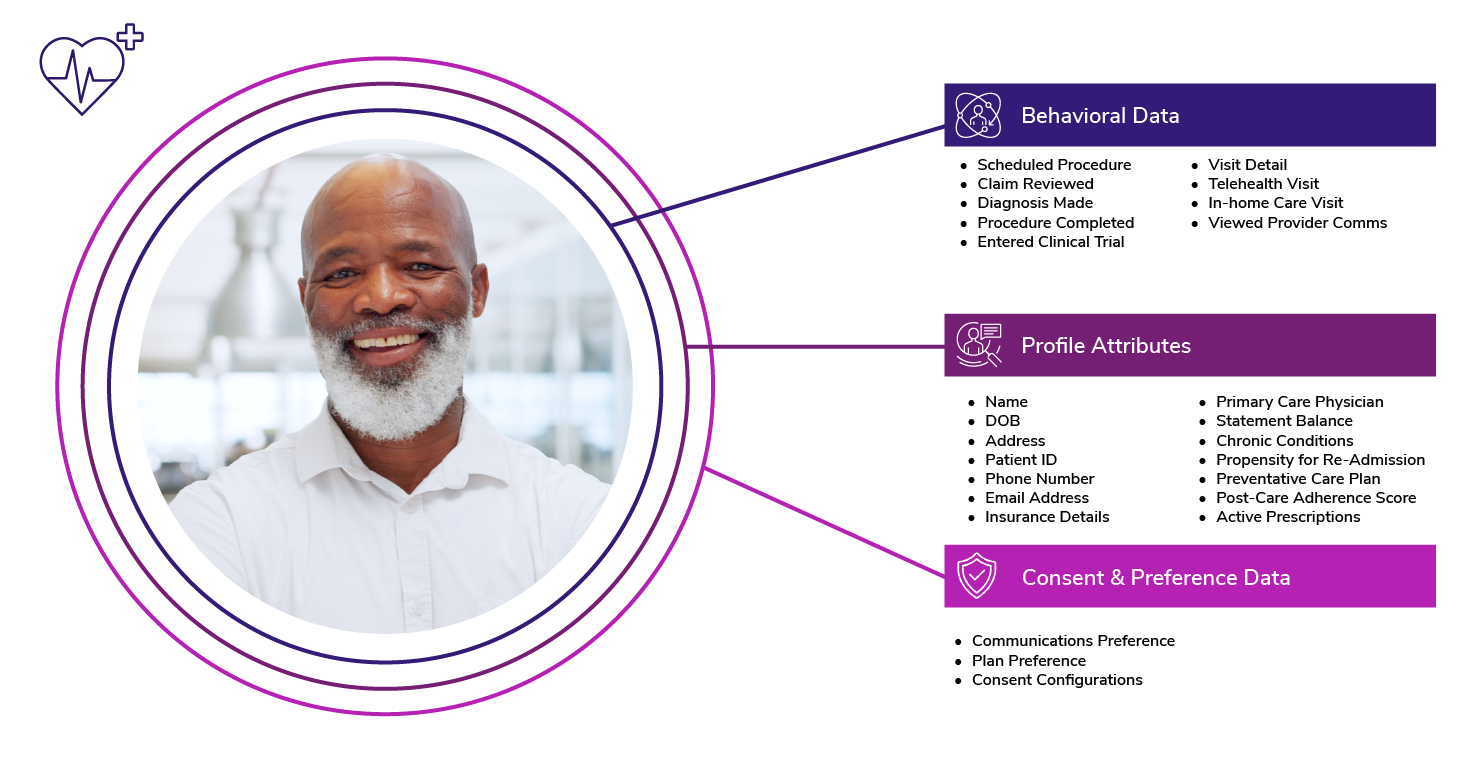
While invaluable, these applications and analyses may be difficult to achieve initially due to the sensitive nature of the underlying datasets required to build the profile. Despite the transformative potential of CDPs, it's crucial for stakeholders to navigate regulatory and ethical considerations diligently, especially with sensitive patient data.
A Two-Step Approach
Given these considerations, some organizations choose a two-step approach to CDP adoption where initial use cases for marketing and de-identified data are prioritized in the short-term (phase 1), while patient and PHI data is ingested in phase 2. A two-step approach ensures organizations achieve value from a CDP more quickly through activating non-sensitive data immediately. Then, once all major acquisition and marketing use cases are underway, the organization can work towards the long-term ambition of ingesting clinical data. This approach may also help with financial buy-in given that CDPs can be a significant investment.
Operational and Controllership Efficiencies
In addition to improving the lives of patients and members, CDPs often result in an internal reduction in duplication of efforts, streamline the work of many disparate teams, and mitigate risks related to privacy & controllership. Efficiencies include:
- A forcing function for a center of excellence and cross-functional collaboration
- Automation and workflow optimization, including streamlining tasks and reducing manual effort regarding audience creation & activation
- Ensure compliance with data protection regulations
- Provide tools for data governance & privacy controls (at the audience and user level)
- Mitigate risks with data breaches as a central source is more easily managed
- Faster tie to insight with actionable data & centralized insights
- Overall operational agility and competitiveness
What to Consider When Evaluating a CDP
Investing in a CDP for digital transformation is often a significant investment, and requires justification for expenditure. A north star vision is often referred to when choosing to adopt a CDP, however when building out an ROI for platform adoption, healthcare organizations should consider several key factors:
- Use Case Readiness - Ensure that the organization has clearly articulated business use cases that speak directly to patient, member, or business outcomes. Use cases should be inclusive of audience, moment, outcome, content, and channel details.
- Pain Point Clarity - In addition to customer-facing use cases, will CDP adoptions solve internal pain points, and how? Is the solution a catalyst or a requirement for the solve?
- Data Quality - A CDP makes use of existing data sources. If the data quality of these sources is low, the activation/outcome of the use cases will not drive value. Evaluate data quality with a comprehensive assessment before ingesting into a CDP or kickstarting a CDP program.
- Tech Stack Integration - Ensure the organization understands the necessary data ingestion inputs and orchestration & activation connections (channels) needed. A comprehensive existing martech and tech stack diagram will kickstart this process.
- Internal Readiness - Getting value from CDP requires significant people resources up front, as well as change management programs post-implementation. Consider the teams that need to be involved in the CDP vendor selection, implementation, and adoption processes. Are IT, data, marketing, product, digital, and other teams on board and with the capacity to give to this program? Are the right skill sets and processes in place?
Fundamentally, a CDP acts as the activation layer to your orchestration strategies. If your organization is unclear on any of the above considerations, we recommend conducting a broader readiness assessment prior to purchasing a solution to ensure value is realized from your investments.
Looking Ahead
CDPs are here to stay, and as the healthcare landscape continues to evolve to support customer preference, the role of CDPs will only grow in significance. Yet, we’ve found that many payers, providers, and healthcare organizations experience difficulty in realizing value from their technology investments. We’ve seen first-hand that some organizations become dissatisfied or disappointed with the velocity of KPI or ROI performance once a CDP has been stood up. Moreover, teams lament around the promises from the technology compared to what has been delivered.
To shorten the time to value for CDP adoption, health organizations must double down on what matters most—investing the time up front to clearly document use cases, ensure data quality, and prepare for internal readiness. Change management and people processes are essential ingredients for CDP success—without them, organizations are left with yet another technology solution that sits on a shelf.
While CDP is not a magic wand for data activation (no single technology is), a CDP can be the catalyst for generating omnichannel, personalized, multi-moment experiences for patients, members, and caregivers. Investing in a CDP when ready will enable marketers and clinicians to make use of patient data more effectively than ever before.
Featured Perspectives

Enabling Personalization at Scale for Healthcare Organizations with a Customer-First Operations Model

Enabling Today’s Healthcare Audiences with Commerce & Self-Service Solutions
